Antimicrobial Resistance (AMR)
What is Antibacterial Resistance?
Antibacterial resistance occurs when an antibiotic agent (drug, chemical, or other substance) can no longer effectively kill the bacterial cells or stop them from multiplying.
Microbes acquire mechanisms to resist the effects of antibiotics. Some of these drug-resistant bacteria may be resistant to multiple types of antimicrobials, and are referred to as “superbugs”.
Antibacterial resistance is not a new phenomenon. Studies of bacteria extracted from arctic permafrost revealed that resistance has been present in nature for more than 30,000 years. Microorganisms naturally produce substances that inhibit the growth of competitor organisms. As a result of selective pressure, some bacterial competitors have evolved cellular mechanisms that combat the antibiotics. In fact, most antimicrobial drugs are derived from microorganisms themselves.
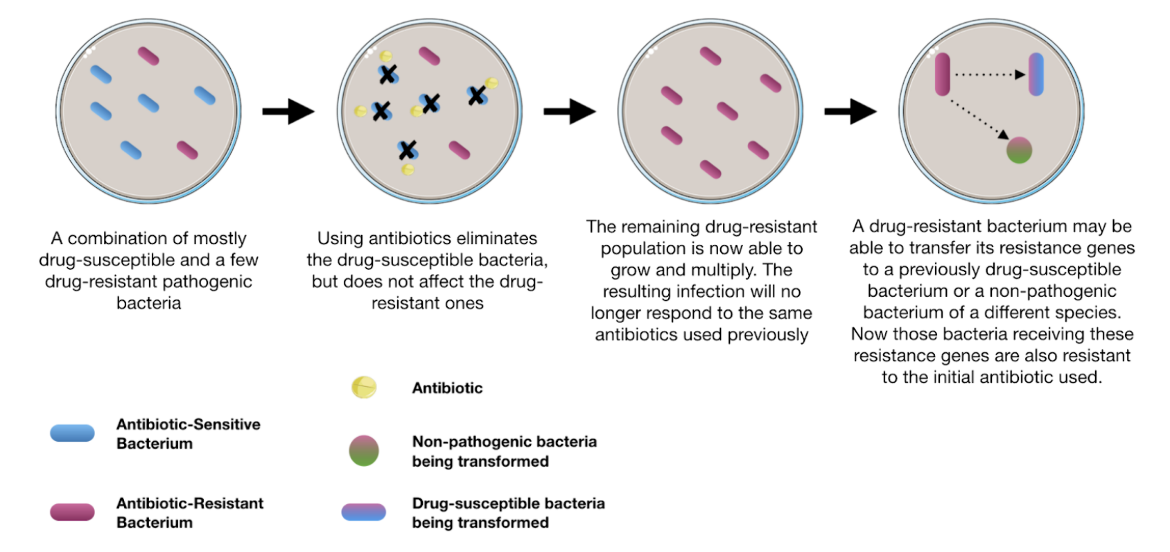
While bacteria are said to possess “intrinsic” resistance to one or more antibiotics, the vast majority of antimicrobial resistance seen today is “acquired resistance,” seen in a previously drug-susceptible population (Munita et al., 2016). Figure 1 illustrates schematically how antibiotic treatment can select for resistant bacteria and how these resistant bacteria can in turn transfer genes conferring resistance to previously susceptible organisms. Once bacteria acquire more than one resistance gene, they can become multi-drug resistant.
|
| Figure 1. Schematic illustration of how antibacterial resistance occurs and spreads. Adapted from (CDC, 2013). |
Why Should We Care about Antimicrobial Resistance?
Discovery of the first antibacterial agent revolutionized modern medicine by providing not only a cure for infectious diseases, but also by enabling other medical advances. Today, antimicrobial agents are essential for the success of surgeries, cancer therapy, organ transplantation, and treatment complications arising from certain chronic diseases (e.g., cystic fibrosis).
Implications of not having access to antibiotics due to antimicrobial resistance could mean that
- many modern medical interventions, such as routine joint replacement surgery, cancer chemotherapy, childbirth, neonatal intensive care, and even international travel may be deemed too risky or no longer possible
- uncontrolled infections may lead to increased hospitalizations, frequent and severe infections leading to limb amputations, increased pain and suffering, and death.
References
Antibiotic Resistance Threats in the United States, 2013. (2013). Retrieved from https://www.cdc.gov/antimicrobial-resistance/media/pdfs/ar-threats-2013-508.pdf?CDC_AAref_Val=https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf
Munita, J. M., & Arias, C. A. (2016). Mechanisms of Antibiotic Resistance. Microbiology spectrum, 4(2), 10.1128/microbiolspec.VMBF-0016-2015. doi:10.1128/microbiolspec.vmbf-0016-2015
March 2025, Gauri Patel; Reviewed by Dr. Tanaya Bhowmick
https://doi.org/10.2210/rcsb_pdb/GH/AMR/about/amr



